
Justice. Mercy. Faith.
Through The Christian Citizen, we seek to shape American Baptists’ and others' minds on matters of public concern by providing a forum for diverse voices living and working at the intersection of faith and politics, discipleship and citizenship.
Featured Articles
What a difference a pronoun can make. And yet, it makes no difference in the true meaning of the description of God. God is like a loving parent.
I have to remind myself that God accepts me apart from my ability or success as a parent or as a leader. As family leaders and church leaders, we don’t always measure up to our own principles. But whether you are a church leader or a family leader or both, God’s grace is present.
Each Friday in The Christian Citizen, we publish a Religion News Roundup with summaries of religion news stories and links for those who want to read more.
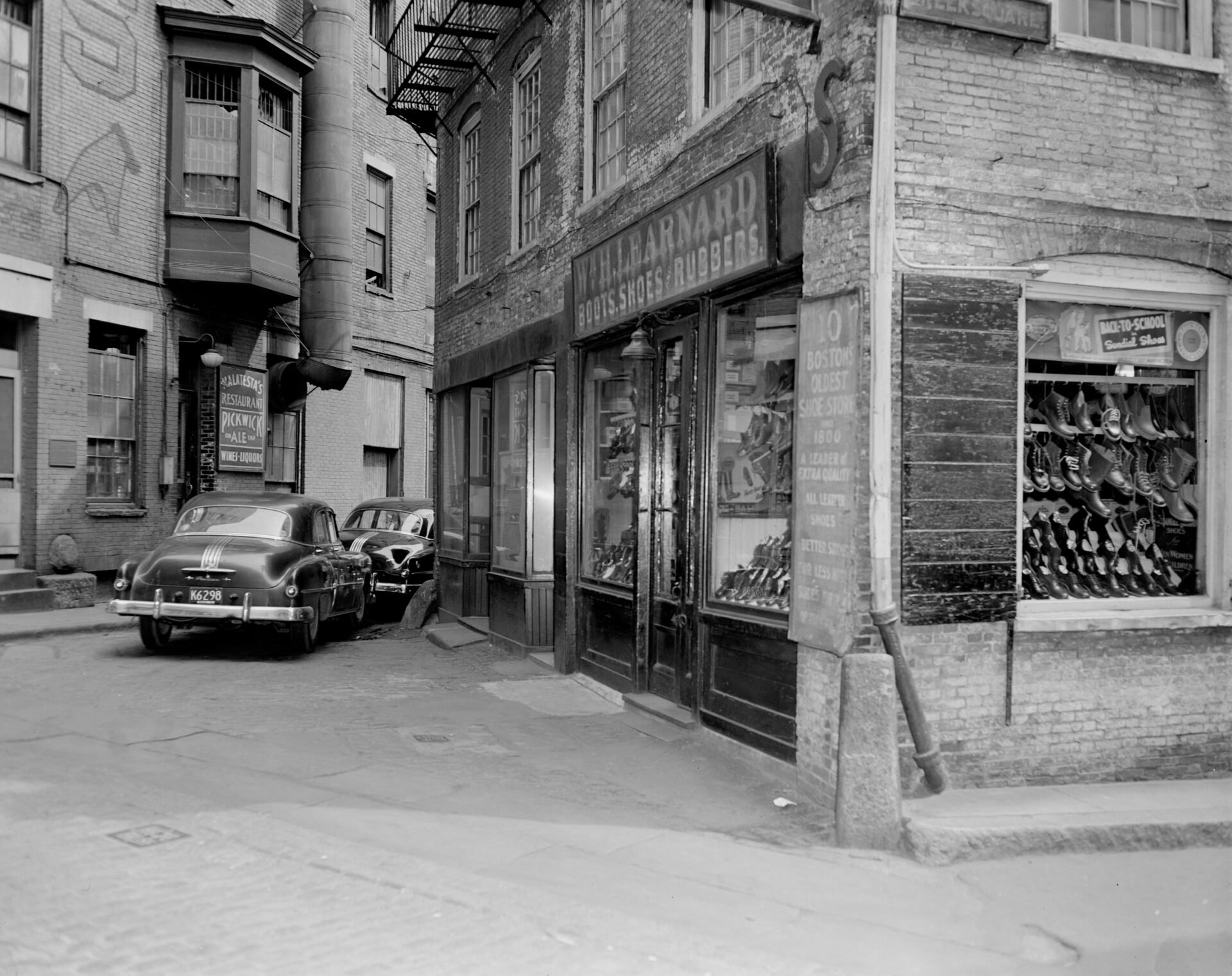
Rev. Wayne Lee realized that if he was called to serve the people of Philadelphia’s Chinatown, he needed to care about what the people cared about. His example of faith pushes against the theological and social boxes that have been drawn for us.
History shows us that plenty of surprises have happened in past papal elections. As we watch for the white smoke above the Vatican, let us pray that the next leader will have the wisdom and guidance necessary to lead the world’s largest group of Christians through the crises that will inevitably mark his pontificate.
Rooted in Heaven * Grounded in Love
*
Rooted in Heaven * Grounded in Love *

Christian Citizen Ambassadors
At The Christian Citizen, we’re passionate about justice, mercy, and faith. We produce award-winning content that is provocative, timely, and relevant. What started more than 25 years ago as a print publication is now a digital-first publication that maintains a commitment to print. More recently, we’ve added a weekly e-newsletter, podcast, and a growing presence on social media. Now, for the first time, we’re adding a member support program—Christian Citizen Ambassadors!
Celebrating AAPI Heritage Month
Rev. Wayne Lee realized that if he was called to serve the people of Philadelphia’s Chinatown, he needed to care about what the people cared about. His example of faith pushes against the theological and social boxes that have been drawn for us.
I suggest that when we encounter a silent story, we needn’t automatically view it as an omission to be mourned or reclaimed but can see it as telling in and of itself, brimming with meaning.
The apostle Paul writes that since we have been reconciled with Christ, we are to become ambassadors for Christ in the world. In Christ, let us also be ambassadors of peace and love in the world in such a time as today.
In early adulthood, I was struck with an epiphany about my identity and heritage. If I believed God to be an intentional God, who has a hand in my very creation and being knit together, then God has an intention in making me who I am in my Chinese Americanness.
Tens of thousands of Marshallese live in diaspora in the United States. Our own church has discovered that sharing space with our Marshallese neighbors has helped us grow spiritually while providing safe space for a displaced people.
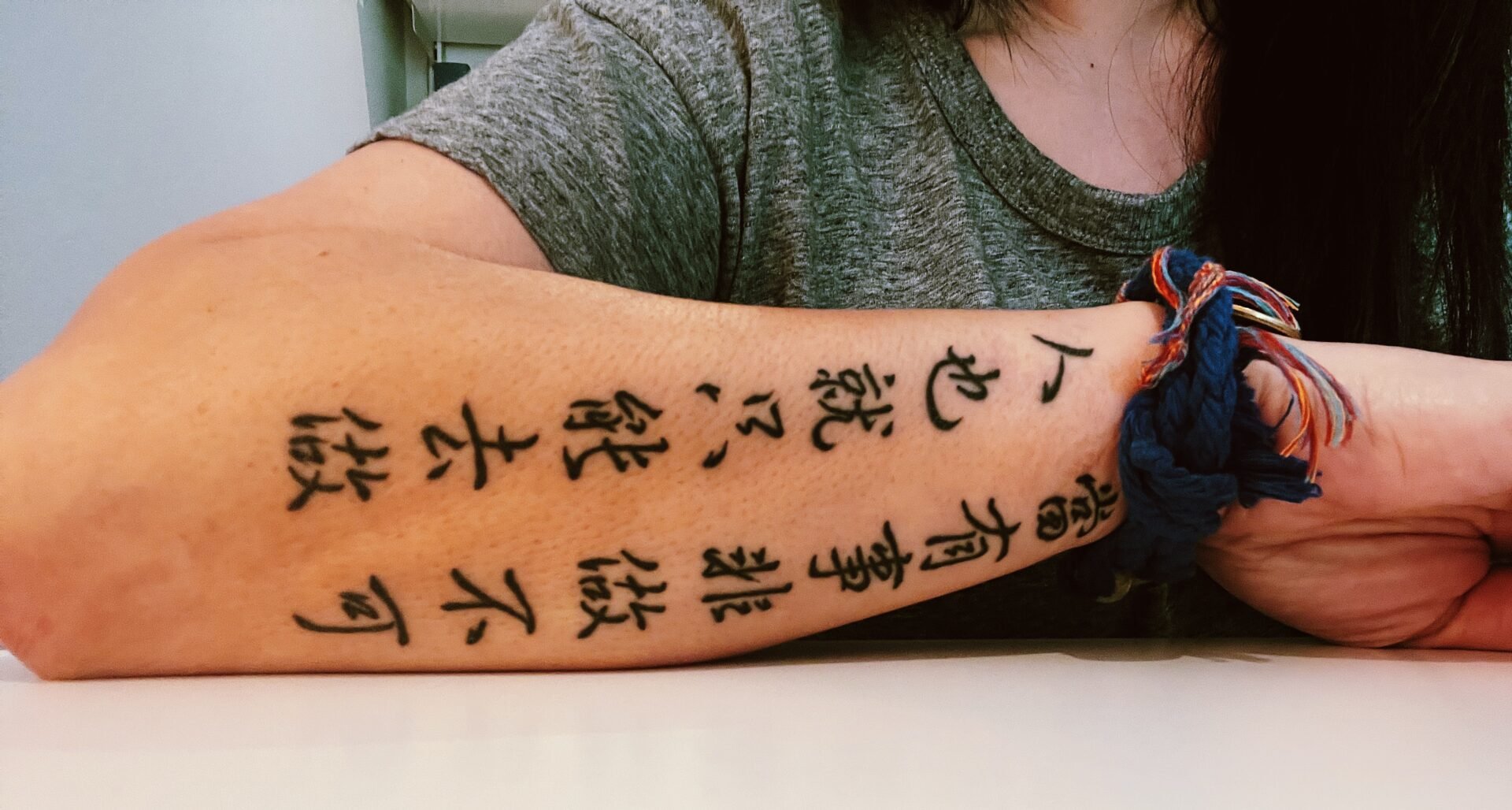
If our bones are alive, if they carry in them strength of our ancestors, trauma of humanity’s transgressions, even predispositions for nutrition… if they—like the Scriptures say—have the capacity to be troubled, to ask questions, to experience restoration, to be reanimated as recipients of God’s ruah (breath), then we have to wonder, what is in our bones?
Discover your own backstory because it will permit you to empathize with others’ backstories. Take time to share your backstory with others, always being mindful to allow time for them to also share theirs.
Wherever we find ourselves to be, together as settlers, refugees, and sojourners, we can become contributing members and citizens of our new home.
National denominational conventions are opportunities to see each other in the flesh and to break down myths, stereotypes, and perhaps our fears of the other. When you see me, I hope that you will not just see me as Don Ng but also see me as an Asian American Pacific Islander person. I will see you too!

Write for us!
We produce thought-provoking articles and inspiring essays that intersect faith, politics, discipleship, and citizenship while examining a variety of public concerns, from gun violence, racism, trauma, and sexual violence to poverty, food insecurity, disabilities, and immigration.












From their diverse backgrounds, the early church discovered inclusion in Christ that led them to equitably share everything that they had among them. Nothing wrong with DEI at Pentecost!